
Starting on a gluten-free and casein-free (GFCF) diet for your clients can result in profound improvements. Many times, that starts with defining for my clients what these things are and in a way that is digestible (see what I did there? ;-))
Gluten refers to the proteins found in wheat, rye, barley, spelt, kamut, and triticale. Gluten helps foods maintain their shape, acting as a glue that holds food together. It can be found in many types of foods, dressings, sauces, and condiments. Casein is a protein found in milk and other dairy products. Similarly to gluten, casein protein can be found in many things, not just dairy products. In this article whether we say gluten-free and casein-free or gluten-free and dairy-free, we are generally talking about the same thing.
I have found that implementing a gluten-free and dairy-free diet can potentially offer a wide range of benefits for many of my clients, both children and adults with varied conditions. For my clients that are children with special needs or developmental delays, improvements can include better receptive and expressive language, enhanced cognition, improved sleep cycles, less hyperactivity, improvements in constipation, and a decrease in disruptive behaviors. In fact, one study found that over a 5 month period, participants on a gluten-free diet showed an improvement on a number of behavioural measures.[1] If you are interested in the science behind a GFCF diet, read my article on 7 science-based reasons a GFCF diet affects the brain and autism.
Consistently following a special therapeutic diet can offer immense benefits for your clients.
But, not every client responds the same way to dietary intervention and sometimes they may wonder why a dairy-free and gluten-free diet is not working for them.
Maybe they thought mood or behavior would improve, or perhaps they were hoping for improvements in digestive symptoms, sleep, rashes, anxiety, hyperactivity, or irritability.
Maybe the diet was working at first, or maybe they never saw the results they were hoping for.
I have heard these challenges in my practice over the last 20 years (you may have as well), and I tell clients and practitioners in my BioIndividual Nutrition Training program that there are a number of things for them to consider that are based on their personalized nutrition needs. I will share my top 10 reasons why a GFCF diet may not be working and offer strategies that can help.
So if you are wondering or your clients are asking the question:
Why is the GFCF diet not working? Or Why is the GFCF diet not working anymore?
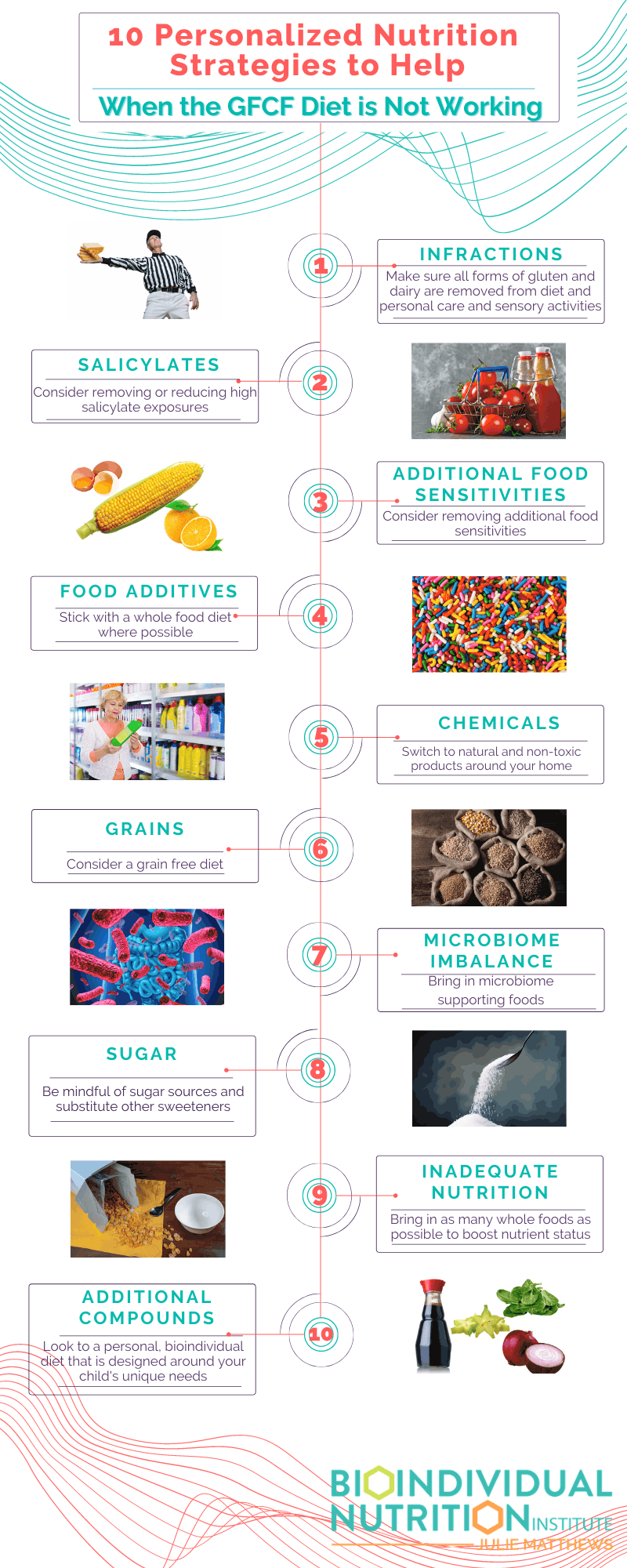
…Here are 10 personalized nutrition strategies to help when the GFCF diet is not working:
1) Infractions
 Firstly, let’s define what an infraction is. It simply means that some small – even minute – amount of gluten protein and/or casein protein is still getting into your client’s diet or can even be absorbed through their skin. This can be from many different sources including:
Firstly, let’s define what an infraction is. It simply means that some small – even minute – amount of gluten protein and/or casein protein is still getting into your client’s diet or can even be absorbed through their skin. This can be from many different sources including:
- Treats or foods at Grandma or Grandpa’s house
- Treats or foods at school or daycare
- Cross-contamination is when a gluten-free and/or casein-free food is sliced, prepared, heated, fried, or placed with foods that contain gluten or casein
- Personal care products like lotions or shampoos
- Craft items like Play-Doh
If your client’s diet is not 100% gluten-free and dairy-free compliant, that can interfere with seeing positive results.
Success Strategy – Keep going. Review your client’s diet, personal care products, even arts and crafts supplies like Play-Doh for gluten and dairy. There can be many names for both of these compounds so make sure they are checking everything.To see the potential gains, they have to be strict so yes, even 1 bite can hurt the progress they are making. And since it takes a while for gluten and dairy to leave their system, being consistent with avoidance – including cross-contamination – is key to success.
2) Salicylates Interfering With Symptom Improvement
 Salicylates are naturally-occurring food chemicals in fruits, vegetables, and other plant foods like herbs, spices, nuts, etc., and in artificial additives and food colorings. So even gluten-free and dairy-free foods can be high in salicylate and if your client is sensitive to these compounds, it could be masking the positive benefits from a gluten-free and dairy-free diet.
Salicylates are naturally-occurring food chemicals in fruits, vegetables, and other plant foods like herbs, spices, nuts, etc., and in artificial additives and food colorings. So even gluten-free and dairy-free foods can be high in salicylate and if your client is sensitive to these compounds, it could be masking the positive benefits from a gluten-free and dairy-free diet.
High salicylate foods can cause headaches, irritability, aggression, anxiety, sleep challenges, urinary frequency and incontinence, gastrointestinal problems, red cheeks or ears (not related to heat), hyperactivity, and other symptoms.
One of the most common experiences I see with clients is that they do a GFCF diet and hope to see improvements in their mood, sleep, and physical symptoms, but they don’t. So they figure “diet,” or a GFCF diet specifically, must not work for them. But instead of giving up, I encourage them to try also removing salicylates. Then, all of the reduction in symptoms and the gains they hoped to see suddenly happen!
It’s important not to give up on diet but to dig deeper! This is where your professional education and training really shines. The tools we teach in our BioIndividual Nutrition Institute allow you as the practitioner to quickly determine who may benefit most from a low salicylate diet and how to guide them through developing a nutritional program best suited for their individual needs.
Some foods that are high in salicylates include:
- Strawberries
- Blueberries
- Raspberries
- Red grapes
- Most melons including watermelon
- Peaches
- Nectarines
- Plums
- Apples
- Red bell pepper
- Cucumbers and pickles
- Ketchup
- Tomato sauce
- Zucchini (with peel on)
- Cinnamon and spices
- Almonds
- Honey
Success Strategy – If your client has implemented a gluten-free and dairy-free diet and is seeing things like the symptoms listed above or irritability, defiant behavior, aggression toward self or others and they are eating many of the high salicylate foods listed above, it may be worth reducing or eliminating those foods as well and assessing how your client feels and behaves as a result. But, it doesn’t mean that the gluten-free and dairy-free diet is not working, it just may mean that there are additional compounds that are also presenting a challenge for your client’s body to process.
3) Additional Food Sensitivities Causing Inflammation
 As a savvy practitioner, you know that when a food causes inflammation in the body there can be many reactions both physically and behaviorally. Removing gluten and dairy, two common food sensitivities, is a great start in reducing inflammation because both of these are frequently inflammatory. Food sensitivities cause inflammation in the body and are specific for each client, so personalizing nutrition based on your client’s particular food sensitivities is important.
As a savvy practitioner, you know that when a food causes inflammation in the body there can be many reactions both physically and behaviorally. Removing gluten and dairy, two common food sensitivities, is a great start in reducing inflammation because both of these are frequently inflammatory. Food sensitivities cause inflammation in the body and are specific for each client, so personalizing nutrition based on your client’s particular food sensitivities is important.
The most common food sensitivities (in addition to wheat and dairy) are:
- Soy
- Corn
- Eggs
- Citrus
- Peanuts
- Nuts
- Chocolate
- Sugar
So once again, if your client has removed all exposure to gluten and dairy and still are not seeing the results that they want, exploring food sensitivities is a good next step.
Success Strategy – Again, have your client stick with a gluten-free and dairy-free diet, but also eliminate specific foods that they are reacting or are sensitive to. And not all food sensitivities are visible like a rash. Sometimes they cause underlying inflammation in the system that you can’t see on the outside, but that affect the brain and get in the way of them seeing improvements.
4) Food Additives
 Chemicals and additives in foods can trigger behavioral issues that can mask the benefits seen from a gluten-free and dairy-free diet. As mentioned above, sometimes the issue is related to salicylates – as in the case of artificial colors – or it can be because of another food compound. Artificial colors, artificial flavors, and preservatives are three very problematic food additives for behavior. Studies show artificial colors and preservatives cause hyperactivity in children. [2]
Chemicals and additives in foods can trigger behavioral issues that can mask the benefits seen from a gluten-free and dairy-free diet. As mentioned above, sometimes the issue is related to salicylates – as in the case of artificial colors – or it can be because of another food compound. Artificial colors, artificial flavors, and preservatives are three very problematic food additives for behavior. Studies show artificial colors and preservatives cause hyperactivity in children. [2]
Another problematic food additive is MSG and related substances high in glutamate. Glutamate is an excitatory neurotransmitter that causes a feeling of excitability and hyperactivity, as well as anxiety, aggression, and other stimulatory sensations – and can be found in food. It is not only found in MSG-type additives such as monosodium glutamate and autolyzed yeast extract, but also in foods naturally high in free glutamate, such as soy sauce, parmesan cheese, and marmite. Glutamate is often found in similar foods high in amines such as sauerkrauts and bone broths.
These food additives can cause a lot of behavior issues that can mask any beneficial results your clients were hoping for with the GFCF diet.
Success Strategy – Cooking a healthy gluten-free and dairy-free diet with as many home-cooked foods as possible is the easiest way to overcome this possible challenge. Reading food labels and knowing exactly what is in your client’s foods is essential. And eliminating food colors, preservatives, and additives is a tremendous step towards the positive improvements you are hoping to see.
5) Chemicals Around The Home
 We don’t often think of chemicals in our clients’ homes interfering with a GFCF diet, because they are not eating these chemicals. However, when they are exposed to them through breathing them in or putting them on their body, they can have detrimental effects.
We don’t often think of chemicals in our clients’ homes interfering with a GFCF diet, because they are not eating these chemicals. However, when they are exposed to them through breathing them in or putting them on their body, they can have detrimental effects.
Synthetic fragrances found in air “fresheners,” candles, fabric softeners, and body care products can also contain salicylates as well as dozens of chemicals that can negatively affect mood, behavior, and brain function. There are many chemicals to be careful of including cleaning products, detergents, antibacterial soaps, flea treatments, and more.
With some of these chemicals your client might see immediate reactions that interfere with diet results; whereas with others, there can be long term damage that your client might not notice right away.
Success Strategy – Educate your client on these chemicals and suggest they avoid them and choose natural options. Pay attention to any chemicals your clients use in their home and encourage them to seek out more natural products. Additionally, suggest that they only put natural body care products on their skin as well. And ask them to be careful of anything they breathe in that could negatively affect their family.
6) Grains Are Irritating The Gut
 Again, the issue of inflammation can be a big one and can mask many of the benefits of a gluten-free and dairy-free diet. Grains and starches can be difficult to digest, especially for some people, such as those with gastrointestinal disorders and microbiome imbalance and can cause irritation – and even inflammation – of the gut, impacting GI symptoms and the microbiome. The gut and brain are closely tied so when the gut is irritated, the brain is often negatively impacted.
Again, the issue of inflammation can be a big one and can mask many of the benefits of a gluten-free and dairy-free diet. Grains and starches can be difficult to digest, especially for some people, such as those with gastrointestinal disorders and microbiome imbalance and can cause irritation – and even inflammation – of the gut, impacting GI symptoms and the microbiome. The gut and brain are closely tied so when the gut is irritated, the brain is often negatively impacted.
If your client is still experiencing digestive symptoms after doing a diet that removes gluten, casein, soy, and any personal sensitivities, a grain-free diet trial may be beneficial. Leaky gut, candida overgrowth, bacterial overgrowth, and other gut imbalances can indicate a benefit to following a grain-free diet.
Success Strategy – The strategy here would be to transition your client from a gluten-free and dairy-free diet to also exclude grains. Most grain-free diets such as the Specific Carbohydrate Diet, GAPS diet, or Paleo also remove starches like potatoes which can be helpful. Many gluten-free products use rice flour, millet, quinoa, or potato as common ingredients. If your client suffers from gut issues (and so many of them do), those grains and starches break down into sugars which can feed those imbalances in the gut. So, by removing grains and starches, you remove the food source for the pathogenic bacteria and fungus, and improve both the gut and the brain.
7) Microbiome Imbalance / Infections
 As we discussed briefly in the section on grains, when your client is experiencing gut issues like leaky gut, dysbiosis (imbalanced bacteria), and gut pathogens, because of the gut-brain connection, it can have a profound impact on your client and their ability to function. While a gluten-free and dairy-free diet is likely helpful, it can be hard to see the effects while the body is also dealing with this other issue.
As we discussed briefly in the section on grains, when your client is experiencing gut issues like leaky gut, dysbiosis (imbalanced bacteria), and gut pathogens, because of the gut-brain connection, it can have a profound impact on your client and their ability to function. While a gluten-free and dairy-free diet is likely helpful, it can be hard to see the effects while the body is also dealing with this other issue.
As we mentioned in diet strategy #6, grain-free and starch-free diets can be helpful with dysbiosis.
Another strategy is a low FODMAPs diet. FODMAPs are fermentable carbohydrates that bacteria feed on and can create gas, bloating, pain, diarrhea, and constipation.
Additionally, a low oxalate diet can be helpful with dysbiosis, as high oxalates damage the microbiome. We’ll talk more about this diet strategy in #10.
Sometimes, more than one diet is implemented and other times people switch to a new diet. But in a vast majority of situations, gluten-free and casein-free are still recommended.
Success Strategy – The strategy here would be to work with your client on supporting the good, healthy gut bacteria by eating a clean, whole foods diet and adding in probiotic rich foods. Sauerkraut, kimchi, homemade dairy-free yogurt, kombucha are just a few things that can be rich in probiotics and can be beneficial to add to the diet while you consider which therapeutic diet or principles might help your client best. If you are a BioIndividual Nutrition Practitioner practitioner, our diet assessment tool helps you hone in on the diet that can be most helpful for your client’s needs.
8) Sugar
 Sugar can be inflammatory, cause behavioral reactions, and even deplete vital minerals. Sugar can create problems in the body which could be interfering with the success of a gluten-free and dairy-free diet.
Sugar can be inflammatory, cause behavioral reactions, and even deplete vital minerals. Sugar can create problems in the body which could be interfering with the success of a gluten-free and dairy-free diet.
Since sugar is inflammatory, it can cause digestive and systemic inflammation that can lead to a worsening of symptoms.
Furthermore, sugar is another compound that can make gut dysbiosis worse. Since the pathogenic organisms feed off of sugar, a diet high in sugar is going to contribute to the growth of those bugs. This can cause behavioral and learning issues which can interfere with the benefits seen from a gluten-free and dairy-free diet.
When your client is undertaking a nutritional intervention, it is important for them to stick to whole, unprocessed, fresh, and organic foods whenever possible and avoid sugar.
Success Strategy – The obvious thing is to reduce or eliminate sugar. This can be done in a few ways. There are other sweeteners which can be enjoyed like coconut sugar that can make the switch easier. They can simply switch out regular white sugar for coconut sugar and slowly begin reducing from there. Coconut sugar has a lower glycemic index, but keep in mind it is still sugar and has negative properties like feeding yeast, so your clients should still use it sparingly. All natural fruit can also be a good alternative to sugar. They can use things like bananas to sweeten smoothies and even muffins. Other sweeteners like stevia or monk fruit can be wonderful alternatives to sugar without the negative health effects of artificial sweeteners. Xylitol and erythritol are other options although some people have GI issues with these forms so start slow.
9) Inadequate Nutrition
 Poor quality food and nutrient deficiency can play a role in behavioral issues, attention or focus, sleep, even things like constipation! So you can see how having foods with low nutritional quality in your client’s diet can cause or exacerbate issues. This goes for gluten-free and dairy-free foods too.
Poor quality food and nutrient deficiency can play a role in behavioral issues, attention or focus, sleep, even things like constipation! So you can see how having foods with low nutritional quality in your client’s diet can cause or exacerbate issues. This goes for gluten-free and dairy-free foods too.
Processed foods are not typically nutrient dense and often have fillers, preservatives, and other chemicals. So when your client transitions to a gluten-free and dairy-free diet, try and have them stick to whole foods, or they could be either continuing the same problems or even creating new ones with these foods.
Success Strategy – Encourage your clients to eat whole foods and cook from scratch! Once they determine what they or their child will/will not eat, batch cooking and doubling (or even tripling!) a recipe to eat later is a valuable tip. Muffins, meats, soups, and casseroles can all be stored in the freezer to be reheated for eating later. This allows them to maximize their time and still eat healthy, home made foods. If they do need to bring in some processed foods, teach them to review those ingredient labels and try and bolster their diet with additional fresh vegetables and fruits in the way of smoothies or other creative ways to get them in. They can continue to slowly reduce the number of processed foods as they further hone their diet.
10) Oxalates, FODMAPs, Histamine, and Glutamate – Additional Food Compounds Irritating The Gut Or Body
 Inflammation can occur even on a gluten-free and dairy-free diet, depending on your client’s unique biochemistry. Things like oxalates, FODMAPs, histamine, and glutamate can be problematic for some individuals.
Inflammation can occur even on a gluten-free and dairy-free diet, depending on your client’s unique biochemistry. Things like oxalates, FODMAPs, histamine, and glutamate can be problematic for some individuals.
Oxalates are inflammatory molecules that inhibit mineral absorption, cause dysbiosis, inflame the gut, and cause oxidative stress and pain.
As mentioned above, FODMAPs are fermentable carbohydrates that bacteria feed on and can create gas, bloating, pain, diarrhea, and constipation. This is obviously no fun!
Histamine is another culprit of inflammation. It is often thought of as related to seasonal allergies and itchy, watery eyes, and sneezing. But foods that are high in or liberate histamine can cause other inflammatory issues on the inside of the body as well. And, if your client is also exposed to pollen or other environmental allergies, their “bucket” for histamine may overflow.
These food compounds can cause inflammation,worsen symptoms, and impede the results of their GFCF diet.
Success Strategy – While a gluten-free and dairy-free diet is a great foundation, removing additional foods or food compounds may also be necessary to get the results your clients are seeking. Understanding your client’s specific dietary needs is important in determining the right personalized nutrition intervention for them. So rather than abandoning dietary intervention, it may be a case of fine-tuning. For example, a low oxalate diet can reduce harmful oxalate levels thereby reducing inflammation and pain. But, it can also be helpful with dysbiosis, as high oxalates damage the microbiome. Removing FODMAPs can reduce GI distress. Reducing high histamine foods during a high pollen time may reduce rashes or stomachaches.
To summarize, here are the 10 strategies to help when the GFCF diet is not working.
Personalized Nutrition for Success
The big takeaway point here is to encourage your clients not to give up. A gluten-free and dairy-free diet is a great place to start for many of your clients. And many clients see tremendous improvement from just that. But, if your client does not, there may be other factors at play or additional foods or food compounds that need to be removed as well.
And this is where taking your clients’ unique needs into account and personalizing nutrition recommendations to the bioindividual needs of the individual is the key. What I’ve learned after working with thousands of clients and practitioners I’ve trained is that for a diet to be most successful, it needs to be tailored to the individual needs of each person. Personalized nutrition, or BioIndividual NutritionTM as I call it, is about taking the specific diet principles your client requires and creating the personalized therapeutic diet plan that’s right for them.
My professional Bioindividual Nutrition Training provides a methodology for determining the best therapeutic diet and personalized nutrition recommendations for your clients, along with all the tools, food lists, and meal plans you need.
References
- Whiteley, Paul, Jacqui Rodgers, Dawn Savery, and Paul Shattock. “A gluten-free diet as an intervention for autism and associated spectrum disorders: preliminary findings.” autism 3, no. 1 (1999): 45-65.
- McCann, Donna, Angelina Barrett, Alison Cooper, Debbie Crumpler, Lindy Dalen, Kate Grimshaw, Elizabeth Kitchin et al. “Food additives and hyperactive behaviour in 3-year-old and 8/9-year-old children in the community: a randomised, double-blinded, placebo-controlled trial.” The lancet 370, no. 9598 (2007): 1560-1567.


