Do you have clients who are experiencing regressions right now? Inflammatory response going haywire, despite their usual dietary patterns? Maybe you work with autism families and they are reporting that their children seem to be going through a yeast flare despite anti-candida diets or maybe even anti-fungal therapy? What about clients reporting skin condition flare ups?
Something to consider at this time of year is histamines! Many practitioners are faced with clients or patients reporting worsening of symptoms related to both environmental and/or dietary sources of histamine.
Common physical manifestations of excess histamine:
- Itchy eyes
- Runny nose
- Sneezing
- Itchy throat
- Headaches – especially migraines
- Rashes
Yet don’t be surprised if your client has none of these either! The histamine can be more locally focused, like in the stomach for example, and cause acid reflux. And for clients with auto-immune conditions, their immune response may be atypical
I had a client with a child with autism for example and her son had no outward symptoms of histamine issues yet saw a flare in yeast every spring/fall. Once my client was made aware of this, they were able to reduce high histamine foods, focus on bringing in natural antihistamines, and they were able to bypass this seasonal yeast flare as a result! It was an answer to a long-standing question of why each year they saw this pattern. Getting an answer, and something to do about it, was a complete win for this family!
The body is usually well-equipped to prevent the build-up of histamine
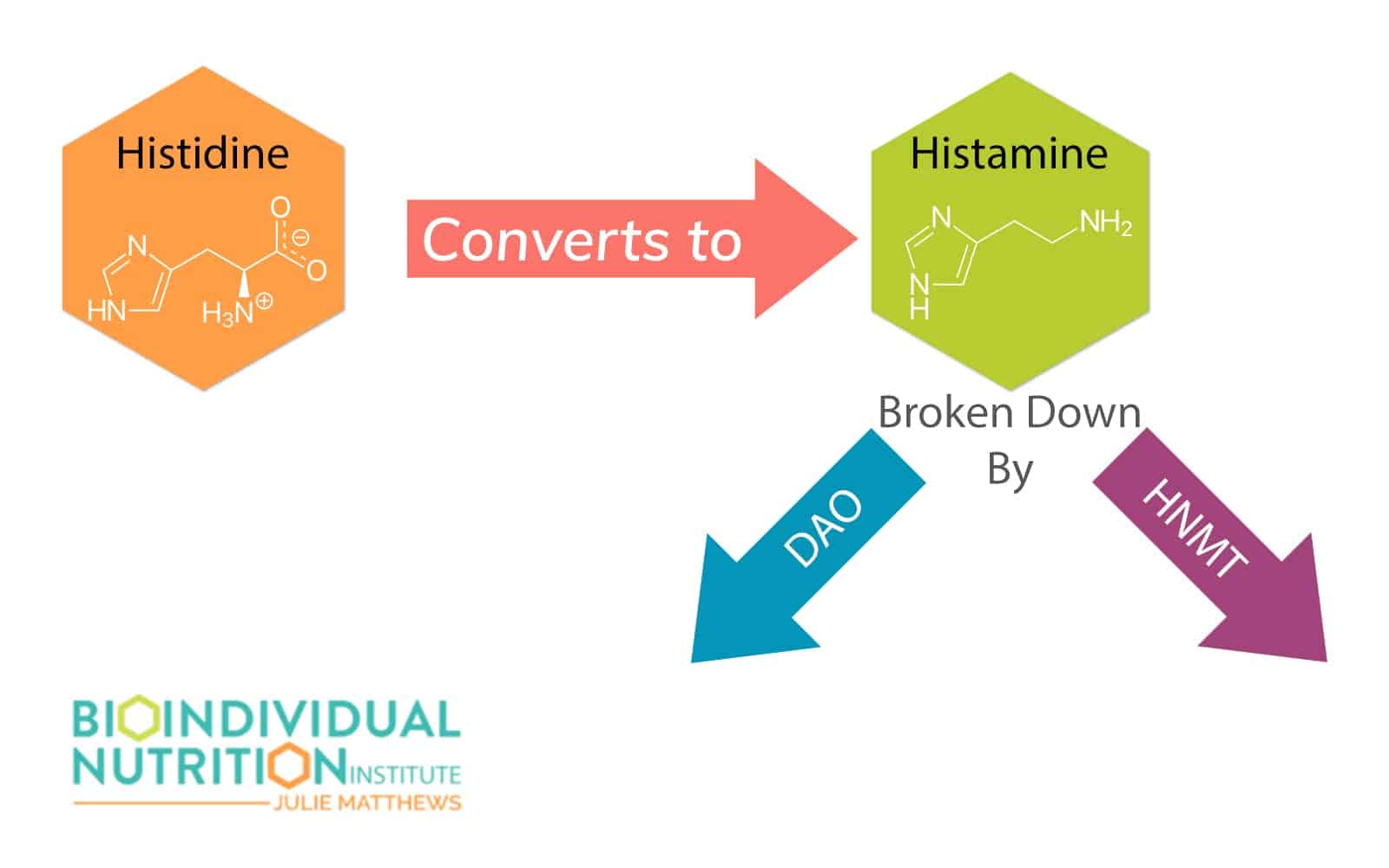
In the body, histamine is enzymatically degraded one of two ways [5]:
- Oxidative deamination by diamine oxidase (DAO) into imidazole acetaldehyde
- Methylation by histamine N-methyltransferase (HNMT) into N4-methylhistamine
However, in some cases, the body may be unable to deal with the histamine produced or consumed either because consumption is too high, or enzymatic activity is too low.
Histamine excess can also place a burden on the immune system so any symptom or condition that is connected with immune function can be impacted by histamine. If you client or patient is expressing that they are experiencing a flare in an inflammatory condition, it is good to ask the following questions.
- Is there a big “bloom” happening in their region now
- Do they live in an area surrounded by greenery/trees
- Have they seen a shift in seasons
- Has it started getting wet and rainy
- Are they eating a diet high in amines, histamines, salicylates, or oxalates
You may have plenty of “gray area” clients who don’t have full-blown Mast Cell Activation Syndrome (MCAS) but who suffer from histamine-related issues each year or as the seasons change. If you do have clients who have mast cell activation syndrome, check out the blog I did on When Histamine Goes Haywire which goes much deeper into the biochemistry of histamine as it relates to MCAS.
So What is a Practitioner to do?
A good clinical assessment is important. Understanding their biggest symptoms or flares can give you the information needed to pinpoint the right nutritional intervention. Then you can look at environmental and dietary patterns that may be contributing to the problem.
Suggesting that your client focuses on lower amine, histamine, and oxalate foods can help calm down the histamine response.
Foods High in Histamine
Histidine is converted to histamine in the body.
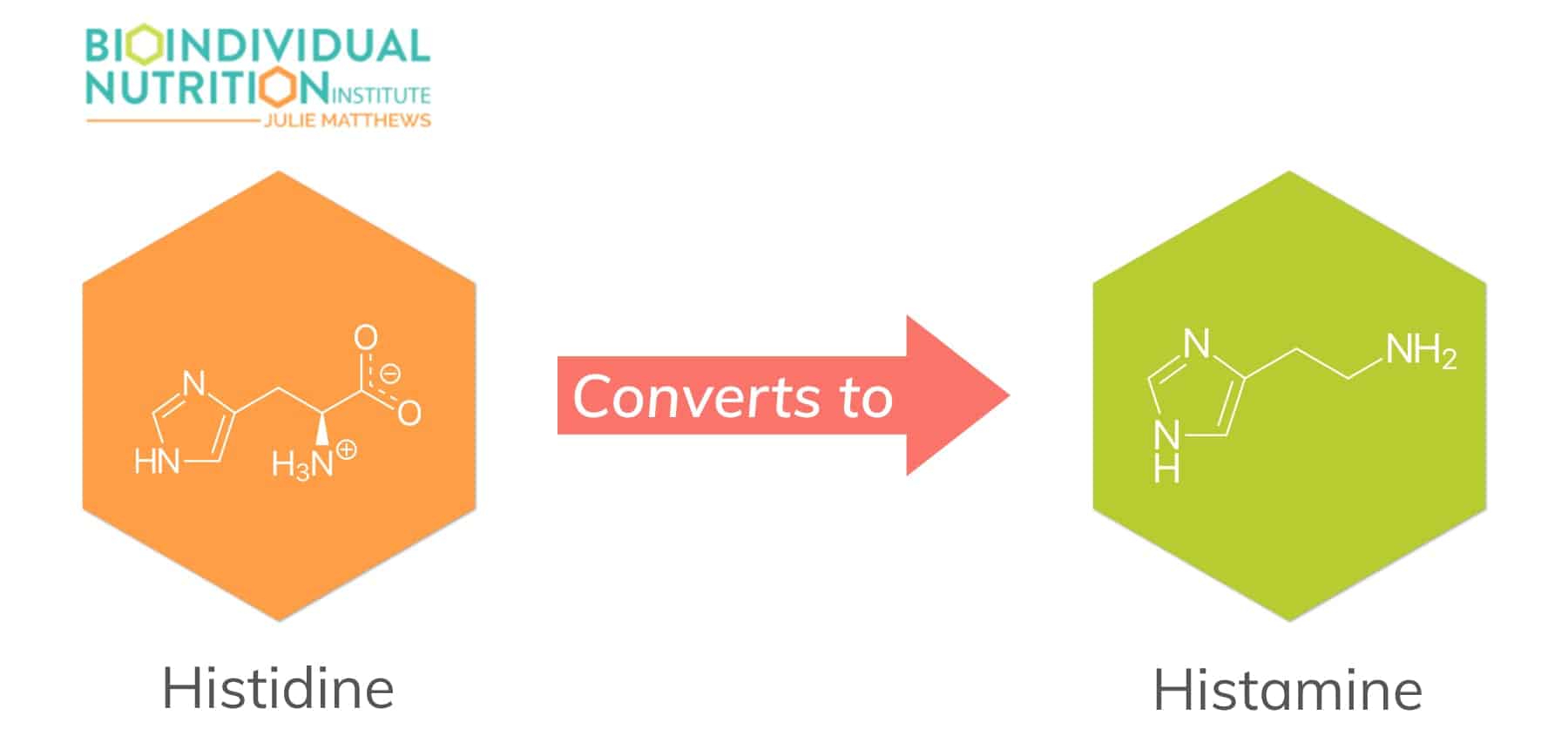
There are several foods high in either histidine, which the body then naturally converts into histamine, or histamine itself. A diet high in histidine rich foods will naturally exacerbate the symptoms and is usually combined with other causes of intolerance, as do histamine rich foods. Fermented foods produced using anaerobic bacteria contain high levels of biogenic amines, like histamine, produced when bacteria break down amino acids. These foods include:
- Fermented dairy products such as matures cheese (cheddar and gouda are very high)
- Other processed dairy products such as yogurt and buttermilk
- Fermented soy products
- Wine and beer and other alcohols
- Processed and cured meats (salami, pepperoni, cured meats, deli meats, sausage)
- The ‘nightshade’ vegetables (tomato, eggplant) and also spinach
- Fermented and pickled foods (sauerkraut, kombucha, pickles)
- Berries contain benzoates which trigger histamine release
- Citrus foods liberate histamine
What is a Low Histamine Diet Trial and Why is it Important
A low histamine diet trial is a trial of low histamine foods and supplements designed to provide the body relief from histamine overload. You can gauge response with this approach and help guide your client through the foods and supplements that may be contributing to high histamine levels. Having them keep track of their foods and note symptoms – reduction or exacerbation – can give you great data in moving forward towards lower histamine levels.
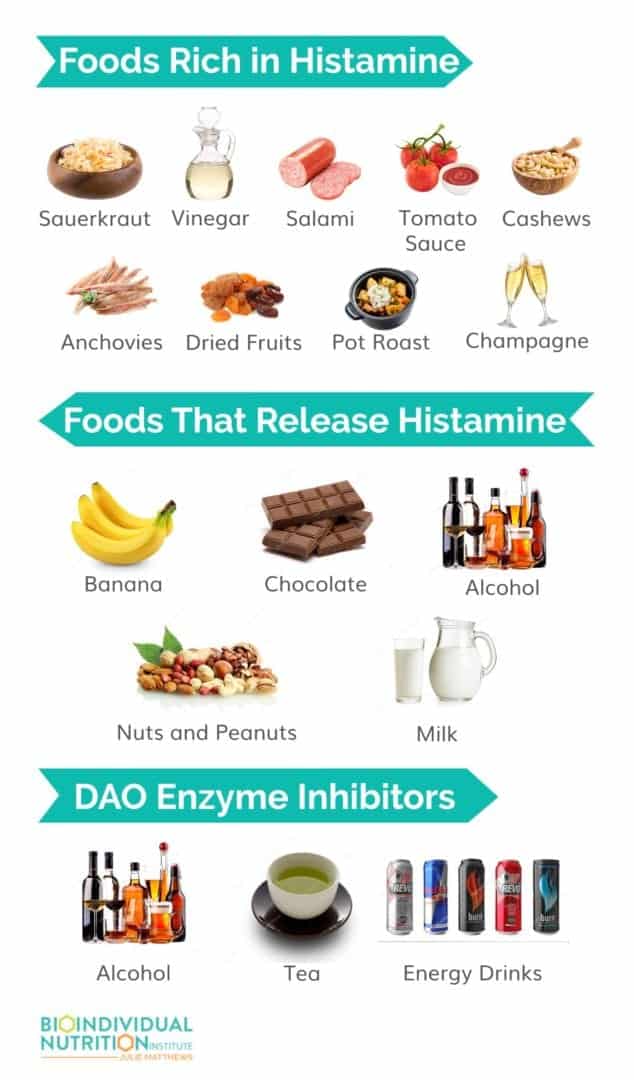
A low histamine diet trial involves the elimination of:
- Foods rich in histamine
- Foods that release histamine
- DAO enzyme inhibitors
Foods Rich in Histamine
- Fermented foods: Sauerkraut, kombucha, fermented dairy including yogurt, kefir, sour cream, soy sauce, fish sauce
- Vinegar and vinegar-containing foods: Pickles, olives, mustard
- Cured meats: Bacon, salami, hot dogs, sausage
- Aged, dried, jerky, smoked and less fresh meat and fish, as well as anchovies and mackerel
- Aged cheese
- Nuts: Peanuts, walnuts, and cashews
- Vegetables: Avocados, mushrooms, eggplant, spinach, and dried tomatoes and tomato sauce
- Dried fruit and citrus fruits
- Long/slow simmered and roasted foods: Bone broths and pot roast
- Fermented alcohol: Wine, beer, brandy, port, sherry, rum, champagne
- Probiotic supplements
Foods That Release Histamine
- Bananas
- Chocolate
- Alcohol
- Milk
- Nuts and peanuts
- Fruit: Papaya, Pineapple, Strawberries
- Tomatoes
- Shellfish
- Artificial preservatives and dyes
DAO Enzyme Inhibitors
- Alcohol
- Tea (black, green, mate)
- Various energy drinks
Low Histamine Foods
- Fresh meats
- Fresh fish
- Vegetables (except spinach, pickles, olives, eggplant, mushrooms)
- Fruits (except bananas, papaya, pineapple, strawberries, citrus, dried fruit, tomato sauce)
- Beans
- Gluten-free grains
- Butter and ghee
But, it may take an even more aggressive approach, which may even include a review of probiotics your client may be taking. Probiotics, while wonderfully supportive for many of our clients, can be high in histamine depending on the strains. Ones to be on the lookout for include:

Probiotic Strains That Contribute to High Histamine
- Lactobacillus casei
- Lactobacillus Bulgaricus
- Streptococcus thermophilus
- Lactobacillus delbrueckii
- Lactobacillus helveticus
Beneficial Probiotic Strains That Help
- Bifidobacterium infantis
- Lactobacillus gasseri
- Bifidobacterium breve
- Bifidobacterium bifidum
- Lactobacillus salivarius
- Lactobacillus rhamnosus (especially GG)
- Bifidobacterium lactis
- Lactobacillus plantarum
For complex cases, reducing even foods higher in salicylate, amines, glutamates, and even oxalates to soothe the inflammatory response.
For the practitioners in my BioIndividual Nutrition Institute, you have access to my comprehensive diets guides for low salicylate, amine, glutamate, and oxalate. These can be wonderful resources for clients looking to reduce their dietary sources. Helping them identify and manage inflammatory responses through nutritional intervention is huge and makes you the most effective clinician you can be!
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6129797/
https://pubmed.ncbi.nlm.nih.gov/16461989/