Gastrointestinal Disorders Prevalence
If you’re a nutrition or health practitioner, you’ve certainly had your fair share of clients with a gastrointestinal disorder or symptoms.
I’m certain of that. That’s because digestive disorders are incredibly common. They affect 60-70 million people in the United States alone. IBS has a prevalence of 15.3 million people, that’s 11.6% in the population.
And the gut is a major factor in health or disease. The gastrointestinal tract is often the first system damaged in chronic disease. We need digestion to break down and assimilate our food and nutrients. Digestive disturbances are common in: neurological disorders, fibromyalgia, chronic fatigue syndrome, skin disorders, autoimmune conditions, and.
And food is a major factor in gut health… as food is in contact with the digestive tract every time we eat. And food can be irritating, inflammatory, and imbalance the microbiome. Or food can be nourishing, healing, and supportive to our beneficial bacteria.
As such, it’s important to know how food affects the gastrointestinal tract and which therapeutic diets can help (which is the purpose of my article today).
But before we talk about special diets, I wanted to share more on the gut-brain connection, as neurological disorders are one of the most common manifestations of GI issues that you’ll likely run into in your practice, if you haven’t already.
The Gut-Brain Connection
The gut and the brain are connected so when the gut is not working well, we can have difficulty with cognitive function and mood.
Let’s take serotonin, for example. Serotonin is a key neurotransmitter in the brain-gut axis. Ninety percent of serotonin is produced in the gut. The microbiome influences the level of serotonin and the functioning of the gut brain axis. It is very important for digestive functioning including motility. And it’s crucial for good mood and happiness When the gut is not working well, neither is the brain.
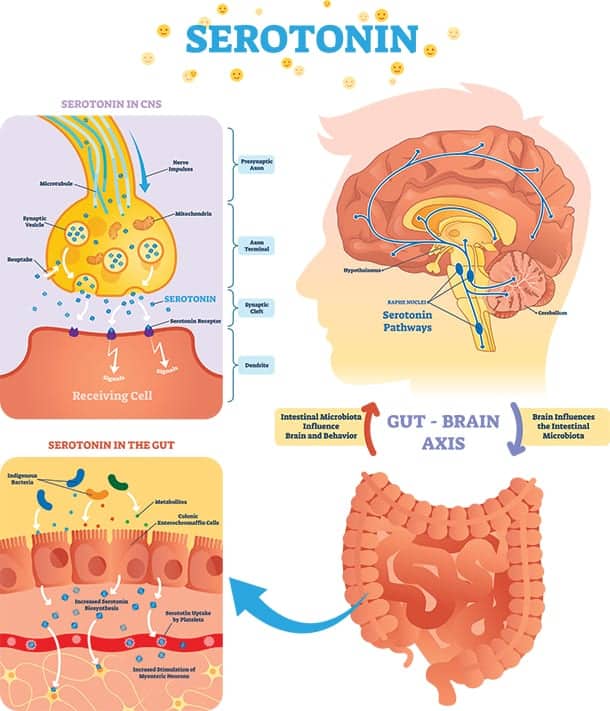
In fact, 30% of people with IBS have depression (vs. 18% of the healthy population), and 16% have anxiety (vs. healthy population).
Digestive disorders are also very common in autism, ADHD, and related developmental disorders.
The good news is: As we heal the gut, neurological disorders improve, often dramatically.
Gastrointestinal Problems and Developmental Delays
Gastrointestinal problems and developmental delays are often connected. According to one study, children with autism, as well as ADHD and other developmental delays, have higher rates of medical conditions than their peers. These medical diagnoses include: diarrhea or colitis, food allergies, asthma, eczema, headaches and earaches.1 It’s a substantive finding, involving a large sample size: 41,000 children aged 3 to 17 years. 5,469 children had one or more of the following diagnoses: autism, intellectual disability, ADHD, learning disability or other developmental delay.
The study found children with developmental disabilities were 3.5 times more likely to have had frequent diarrhea or colitis during the past year. As well as 1.8 times more likely to have had a food allergy during the past year. They were also significantly more likely to have skin allergy, asthma, ear infections, and severe headaches.
When they compared the developmental disability groups to each other they discovered: “Children with autism were twice as likely as children with ADHD, learning disability or other developmental delay to have had frequent diarrhea or colitis during the past year. They were seven times more likely to have experienced these gastrointestinal problems than were children without any developmental disability.”
These findings are important because parents are routinely told one has nothing to do with the other. However, the gut and brain are closely connected, such that the gut is often called “the second brain.”
When the gastrointestinal system is not functioning properly, children and adults struggle with mood, behavior, focus, and thinking.
Your client may not be able to:
- Break down and absorb nutrients properly, leading to deficiency that can affect cognition, mood, and behavior.
- Digest the protein in wheat, dairy, and soy, which form opioid (morphine-like) compounds that negatively affect attention, learning, and behavior.
- Maintain a healthy gut microbiome – pathogenic microorganisms can negatively affect our neurotransmitter levels and cause hyperactivity, aggression and other mood related symptoms.
One of the most important ways to address digestive issues is to look at the foods that are going into the gastrointestinal tract: i.e. “the diet.”
Also there are supportive supplements and other nutritional tools that can help your client:
- Digestive enzymes – digests food to relieve the burden on digestion and help reduce irritation.
- Probiotics – helps supply needed beneficial bacteria.
- Prebiotics – feeds the growth of beneficial bacteria.
- Anti-inflammatory supplements – reduces inflammation throughout the body for symptom relief and healing of the gut.
But without looking at the food going in and whether it’s causing inflammation, harm, and havoc to the underlying biochemistry and system, we cannot make full progress and help your clients improve their health.
Some foods are generally inflammatory to most humans like gluten, for example.2 Whereas others – most grains, salicylates or oxalates – are only a problem for certain people based on their bioindividual circumstance.
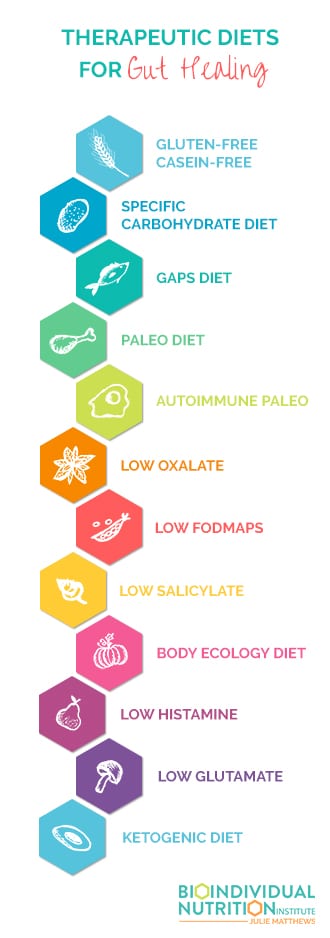
Problematic Foods and Therapeutic Diets for Gut Healing
Some of these strategies are more advanced and others more introductory. I’ll start with the foundation stones for families at the beginning of their journey before covering other diets that can be helpful for more diet-experienced individuals.
Gluten-Free, Casein-Free and Soy-Free Diet
 Gluten, found in wheat and other grains, casein, found in dairy, and soy are all inflammatory proteins. The proteins are hard to digest, and when not properly broken down can form opiate compounds. Opiates (just like morphine) can slow motility of the gut causing constipation and further digestive discomfort, and cause inflammation. Constipation is very common with dairy intolerance – one study of children with constipation revealed that 80% of the patients had a cow’s milk allergy. 3 A gluten-free, casein-free and soy-free diet is a great diet to start with when chronic digestive issues are present.
Gluten, found in wheat and other grains, casein, found in dairy, and soy are all inflammatory proteins. The proteins are hard to digest, and when not properly broken down can form opiate compounds. Opiates (just like morphine) can slow motility of the gut causing constipation and further digestive discomfort, and cause inflammation. Constipation is very common with dairy intolerance – one study of children with constipation revealed that 80% of the patients had a cow’s milk allergy. 3 A gluten-free, casein-free and soy-free diet is a great diet to start with when chronic digestive issues are present.
Grain-Free Diets
 Grains are hard to digest, as they require large amounts of carbohydrate digesting enzymes. And we know that people with autism are often low in the correct enzymes.4 The starch in grains also feed pathogens and small intestine bacterial overgrowth (SIBO), resulting in irritation and damage to the gut, causing diarrhea, constipation, pain, and distress.
Grains are hard to digest, as they require large amounts of carbohydrate digesting enzymes. And we know that people with autism are often low in the correct enzymes.4 The starch in grains also feed pathogens and small intestine bacterial overgrowth (SIBO), resulting in irritation and damage to the gut, causing diarrhea, constipation, pain, and distress.
There are several grain-free diets that can be helpful with digestive problems:
- Specific Carbohydrate Diet (SCD)
- GAPS Diet
- Paleo Diet
Low Salicylate Diet
 Salicylates occur in plant foods, including berries, grapes, tomatoes, almonds, herbs, and spices. But salicylates are also present in honey. In addition to behavioral symptoms, salicylates can cause digestive symptoms such as diarrhea, and can increase digestive pain when consuming FODMAPs.5 6
Salicylates occur in plant foods, including berries, grapes, tomatoes, almonds, herbs, and spices. But salicylates are also present in honey. In addition to behavioral symptoms, salicylates can cause digestive symptoms such as diarrhea, and can increase digestive pain when consuming FODMAPs.5 6
Low salicylate diets include:
- Feingold diet
- FAILSAFE diet
Low Oxalate Diet
 Oxalates are inflammatory molecules that are found in certain foods, including: Nuts, spinach, Swiss chard, chocolate, and beans. Oxalates can kill good bacteria and perpetuate yeast and gut microbiome imbalance. And create inflammation in the gut.
Oxalates are inflammatory molecules that are found in certain foods, including: Nuts, spinach, Swiss chard, chocolate, and beans. Oxalates can kill good bacteria and perpetuate yeast and gut microbiome imbalance. And create inflammation in the gut.
Low FODMAPS Diet
 FODMAPS is an acronym for various fermentable carbohydrates including oligosaccharides found in the onion family and polyols found in prunes. Fermentable carbohydrates feed bacteria, but when there is an imbalance such as small intestine bacterial overgrowth (SIBO) it can cause gas, bloating, pain, diarrhea and constipation. Studies have shown a Low FODMAPS diet can be helpful for IBD.7
FODMAPS is an acronym for various fermentable carbohydrates including oligosaccharides found in the onion family and polyols found in prunes. Fermentable carbohydrates feed bacteria, but when there is an imbalance such as small intestine bacterial overgrowth (SIBO) it can cause gas, bloating, pain, diarrhea and constipation. Studies have shown a Low FODMAPS diet can be helpful for IBD.7
Body Ecology Diet
 The Body Ecology diet avoids sugar and foods that feed and perpetuate candida overgrowth, and includes foods that are healthy – while supplying good bacteria through fermented foods. It’s often used to address candida overgrowth and other “inner ecology” imbalances.
The Body Ecology diet avoids sugar and foods that feed and perpetuate candida overgrowth, and includes foods that are healthy – while supplying good bacteria through fermented foods. It’s often used to address candida overgrowth and other “inner ecology” imbalances.
Low Histamine Diet
 There are a variety of low amine and histamine approaches. As the name implies, histamine is one type of amine. You find amines in: bone broth, sauerkraut, fermented foods, wine, beer, chocolate, and cheese. Histamine and other amines can cause intestinal and systemic inflammation, diarrhea, and abdominal cramps.
There are a variety of low amine and histamine approaches. As the name implies, histamine is one type of amine. You find amines in: bone broth, sauerkraut, fermented foods, wine, beer, chocolate, and cheese. Histamine and other amines can cause intestinal and systemic inflammation, diarrhea, and abdominal cramps.
Low Glutamate Diet
 Glutamate is an excitatory neurotransmitter – think the opposite of calm! Glutamate is often present in food. Glutamate often occurs in similar foods to histamine like: sauerkraut, fermented food, bone broth – and occurs in high amounts in soy sauce and parmesan cheese, and additives like monosodium glutamate (MSG) and autolyzed yeast extract. Glutamate can affect the nervous system and can cause reactions such as inflammation systemically. Glutamate can also cause diarrhea, constipation, and gut issues.
Glutamate is an excitatory neurotransmitter – think the opposite of calm! Glutamate is often present in food. Glutamate often occurs in similar foods to histamine like: sauerkraut, fermented food, bone broth – and occurs in high amounts in soy sauce and parmesan cheese, and additives like monosodium glutamate (MSG) and autolyzed yeast extract. Glutamate can affect the nervous system and can cause reactions such as inflammation systemically. Glutamate can also cause diarrhea, constipation, and gut issues.
Ketogenic Diet
 The Ketogenic diet is a very low carbohydrate diet that uses ketones/fat for energy instead of glucose/sugar. Though very restrictive, keto can help with balancing the microbiome and supply the proper energy for the gut to heal for the right individual. Remember, this diet is very strict and high fat diets can often lack the beneficial fiber for the microbiome – so more studies are needed to find out when this diet supports or imbalances the microbiome. 8
The Ketogenic diet is a very low carbohydrate diet that uses ketones/fat for energy instead of glucose/sugar. Though very restrictive, keto can help with balancing the microbiome and supply the proper energy for the gut to heal for the right individual. Remember, this diet is very strict and high fat diets can often lack the beneficial fiber for the microbiome – so more studies are needed to find out when this diet supports or imbalances the microbiome. 8
Underlying Considerations for Choosing a Special Diet
Now that you know a little about the diets, let’s tackle four considerations that arise with gut health, including their potential implications, and possible dietary choices for these gastrointestinal issues.
Inflammation
Inflammation affects the gut by aggravating the gut wall, causing leaky gut, leading to food sensitivities, and often contributing to chronic disease or autoimmunity, affecting every system. Symptoms can include diarrhea, constipation, gas, bloating, and pain.
Dietary considerations: Food allergies and sensitivities, oxalates, salicylates, amines, histamine, FODMAPs, and grains.
Mitochondrial dysfunction
Mitochondria are the powerhouses of the cell responsible for making energy, and if they aren’t functioning well, it can lead to constipation, but also fatigue, pain, and disease in any organ or system of the body.
Dietary considerations: oxalates, a ketogenic diet, or adequate carbohydrates.
Poor sulfation
Sulfation is a set of biochemical processes that use sulfate, and it’s a necessary process for intestinal barrier integrity (to avoid leaky gut) and aid digestion. An imbalanced gut microbiome can contribute to poor sulfation. Poor sulfation can cause reactions to phenols, salicylates, and amines – many are present in foods traditionally considered “healthy” like berries, spices, almonds, fruits and vegetables.
Additionally, when sulfate the building block for sulfation is low, problems with oxalates can result,
Dietary considerations include salicylates, amines, and other phenols, plus oxalates.
Microbiome imbalance
Good bacteria is essential for good digestive health, while pathogens contribute to digestive issues and disease. Eating a diet that supports good bacteria while starving out the bad pathogens can be tricky to balance. For example, high fiber foods are good for beneficial bacteria but cause reactions for clients with SIBO. Additionally, if there is an imbalanced microbiome these reactions to foods that might otherwise be healthy can result in reactions to salicylates, amines or oxalates.
Dietary considerations include: FODMAPS, salicylates, oxalates, and amines.
The key is eating foods that support digestion and feed beneficial bacteria, while not causing another reaction. Determining which foods your client or patient needs while avoiding those that cause or contribute to underlying problems is essential to helping them improve.
Understanding the Relationship Between Symptoms and Foods
Complicating matters further, practitioners often recommend many healthy foods for “gut healing diets” – such as bone broth, sauerkraut, spinach, and almonds. Such foods contain natural food compounds that can cause or exacerbate the exact GI issue the practitioner is working to resolve!
So as a practitioner, it’s important to understand the big picture of diets and gut health for your client.
Understanding the relationship between symptoms and foods will allow you to help your clients find the right healing diet.
Of course, if you are looking to take your knowledge to the next level, check out our BioIndividual Nutrition Training program.
Share what diet strategies have helped you help your clients – I love to hear success stories!
Explore Enrollment into the BioIndividual Nutrition Training
…CLICK THROUGH….
References:
- https://www.ncbi.nlm.nih.gov/pubmed/22119694
- https://www.ncbi.nlm.nih.gov/pubmed/24533607
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3533146/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3174969/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3388522/
- https://www.ncbi.nlm.nih.gov/pubmed/16247191
- https://www.ncbi.nlm.nih.gov/pubmed/28244679
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5009541/ [Animal study]


