In the past, oxalate research was relegated to kidney-related disorders. Now much more is known.
Whether your interest is autism, cancer, chronic pain, autoimmunity, or generalized inflammation, understanding the role dietary oxalates can play is critical for your clients.
Inflammasome activation is a new discovery related to the immune system and oxalate – which can have some significant implications, especially with age-related disorders and chronic conditions.
What is the inflammasome? It is an innate part of the immune system involved with creating inflammation. It is now known that oxalate can tigger it. The inflammasome has been implicated with several age-related disorders including gout, type 2 diabetes, obesity, cancer, and neurodegenerative and cardiovascular disorders, [1] as well as autoimmune conditions.
So as we begin to understand a broader picture of the various ways high oxalates can be detrimental to optimal health, we can see how/why a low oxalate diet can be helpful for our clients.
Here is some of the latest research. The first study is on the inflammasome. The second is on oxalate and breast cancer, and we just mentioned the inflammasome connection to cancer. The final two research papers are on autism including a study on autism and oxalate, and a paper on diet for autism including the recommendation of a low oxalate diet.
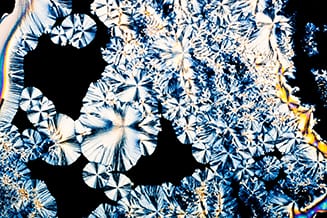
Oxalate Triggers the Inflammasome
 A review of the current literature surrounding oxalates and inflammasome activation is compelling.
A review of the current literature surrounding oxalates and inflammasome activation is compelling.
In this scientific paper, researchers explain how when the body is burdened with oxalates (either through diet or endogenous production) the kidneys can be damaged by the build up. When this happens, blood levels of oxalate rise even more which can activate the inflammasome.
Researchers pointed out how reducing dietary oxalate is important in reducing inflammation that stems from inflammasome activation. In fact, the authors conclude: “Accordingly, inhibiting oxalate-induced inflammasome activation, or lowering plasma oxalate, may prevent or mitigate progressive renal damage in CKD, and also reduce morbidity and mortality due to systemic inflammation.”
Given that the inflammasome is associated with gout, type 2 diabetes, obesity, cancer, autoimmune conditions, and neurodegenerative and cardiovascular disorders it is critical for practitioners to understand the effects oxalate can have on the body, the inflammatory process, and disease, and the important role a low oxalate diet plays. With this new research, oxalates become even more important to consider when working with patients or clients facing age-related conditions involving the inflammasome.
Breast cancer and oxalates – is there a link?
 Research has tied excess oxalate build-up to breast cancer.
Research has tied excess oxalate build-up to breast cancer.
Two types of mice were involved in this study, namely BALB/c or BALB/c nude female mice. BALB/c mice had a wild type immune system.
The researchers found that injecting oxalates in the mammary fat pad region of BALB/c nude mice favored the growth of breast tumors. More specifically, the scientists reported that oxalates promoted the growth of MCF-7 and MDA-MB231 breast cancer cell lines as well as the normal breast cell line, MCF10A.
Moreover, the higher the oxalate concentration, the faster the breast tumors developed.
Interestingly, injecting oxalates in the animals’ back did not induce cancer suggesting that oxalates may cause only breast cells to proliferate abnormally.
BALB/c mice were also injected with oxalates but did not develop tumors although some of the animals did experience some swelling in the mammary fat pad area. Since this swelling disappeared within 24 to 48 hours, this could indicate that the oxalate may have triggered tumor formation, but the immune system of BALB/c mice was strong enough to destroy the cancer cells.
Given this new research, the potential role of oxalate in cancer should be researched much more extensively. And the use of a low oxalate diet and nutritional approach should be studied as well.
How ascorbic acid may cause oxalate nephropathy
 In this case study, a 69-year-old patient with benign prostate hyperplasia and small bowel resection presented with reduced urinary output, fatigue, and trouble speaking. The patient had been taking 2g of ascorbic acid daily for the past 2 years.
In this case study, a 69-year-old patient with benign prostate hyperplasia and small bowel resection presented with reduced urinary output, fatigue, and trouble speaking. The patient had been taking 2g of ascorbic acid daily for the past 2 years.
Since his creatinine and blood urea nitrogen remained elevated, he had to undergo 4 sessions of hemodialysis on the fifth day of admission.
A renal biopsy was performed to identify the cause of this patient’s acute kidney failure. The sample revealed presence of edema, tissue thickening and scarring, and inflammation. Calcium oxalate crystals were also present.
The study authors explain that:
- Ascorbic acid in doses above 2g/day can cause oxalate crystals to deposit in the kidney. This can cause oxalate nephropathy which refers to oxalate-induced damage to delicate structures within the kidney. Nephropathy can eventually result in kidney failure.
- The benign prostate hyperplasia caused chronic urinary retention which probably increased crystal deposition in the kidney.
- Small bowel resection can also increase oxalate absorption by impairing fat absorption in the gut. Reduced dietary fat absorption can cause calcium to bind to fatty acids that aren’t absorbed. This reduces excretion of calcium oxalate in the feces.
Oxalates and Autism
 Researchers studied oxalates in autism, and they measured a 2.5-fold greater level of oxalates in the urine, and a three-fold greater level of oxalate in the plasma, in children with autism.
Researchers studied oxalates in autism, and they measured a 2.5-fold greater level of oxalates in the urine, and a three-fold greater level of oxalate in the plasma, in children with autism.
Their finding was specifically, hyperoxaluria; a condition of high oxalate.
It’s significant to note that the study on autism and oxalate excluded the following groups from their selection criteria: those on a special diet, those with a history of seizures or antibiotic use, those with gastrointestinal disease (in addition to those with kidney stones). This is important to note, because all of these can be conditions of or cause hyperoxaluria.
The study’s selection criteria (omissions) may affect an underrepresentation of the range of oxalate (plasma and urinary) that would occur in a full range of autistic patients. Even with the exclusions, significant oxalate issues were identified. This warrants further study, without excluded variables, to investigate how results may differ. If these groups had been included, rates and levels of oxalate would most likely be even higher.
The study concluded that: “hyperoxalemia or hyperoxaluria may be involved in the pathology of autism spectrum disorders in children.” 1 It then continues to explain that based on the high oxalate finding, certain treatment options, such as a low oxalate diet, probiotic therapy, possibly with Oxalobacter formigenes, and a variety of supplementation may be helpful in these children.
Oxalates are significant in autism because clinically we see a great deal of oxidative stress, considerable inflammation, mitochondrial damage or dysfunction, as well as faulty sulfation and seizures—areas where oxalates can wreak havoc. The discovery and clear indication that high oxalate may be involved in the pathology of autism is both significant and hopeful. This research and the biochemical connections we are highlighting provide further hope and direction for helping children with autism.
Dietary and therapeutic strategies for inflammation in autism spectrum disorders.
 Brain development and function can be influenced by the environment, gut health, and diet in utero and after the child is born.
Brain development and function can be influenced by the environment, gut health, and diet in utero and after the child is born.
This is particularly important in autism. In this article entitled, “Interplay Between Peripheral and Central Inflammation in Autism Spectrum Disorders: Possible Nutritional and Therapeutic Strategies” the authors reviewed diet, nutrition, and other interventions such as probiotics and fecal transplants for helping individuals with autism. I am excited to see two diets that I have found very helpful in my nutrition practice for children with autism on this list: the low oxalate diet and the Specific Carbohydrate Diet (SCD).
In the paper, they explain how lab studies indicate that offspring of mothers who were obese during pregnancy were more likely to develop social communication impairment and repetitive behavior. Scientists explain that the low-grade inflammation caused by obesity could impair the brain’s neuronal circuit which controls behavior in the offspring.
Moreover, anything that adversely influences the development of the gut microbiome (such as the mode of delivery, stress, antibiotics, and diet) will also affect the gut-brain axis. Since gut microbes produce neurochemicals that play a role in social cognition, emotion, and behavior, improving gut health during pregnancy could decrease risks of ASD in the offspring.
As such, they discuss the following promising adjuvant therapies for ASD including:
- A gluten-free and casein free diet – this free step-by-step guide can help you get started
- The Specific Carbohydrate Diet
- A diet low in oxalates
- Adequate intake of micronutrients such as carnitine, zinc, selenium, vitamins A, D, E, and B-complex and omega-3s and omega-6s from real foods and/or high-quality supplements
- Prebiotics and probiotics from the Lactobacillus and Bifidobacterium genus
- Fecal transplants which involve transferring fecal microbiota from healthy donors to an unhealthy individual
While grain-free diets like SCD have gained attention in recent years, the low oxalate diet has been slow to become mainstream nutrition knowledge. So I’m thrilled to see it gaining traction in the nutrition world. I hope researchers continue to study this important diet for gut health, neurodevelopmental disorders, and many other conditions.
Conclusion
Tailoring the right nutritional guidance for your clients or patients is important. As we can see through these studies. elevated oxalate can have a big impact on inflammation, oxidative stress, kidney function, mitochondrial function, and even cancer. Having a clear understanding of how (and when) to safely guide clients and patients through transitioning to a low oxalate diet can make all the difference in their lives.
To learn more on personalized nutrition and therapeutic diets, like the low oxalate diet, and how to use them in your practice as part of a BioIndividual Nutrition® plan, explore my BioIndividual Nutrition Training.


