Do you experience random headaches? Or perhaps your tongue gets all swollen when you eat tomatoes?
As you’ll discover in this article, these symptoms aren’t ‘all in your head’ but could be related to how your body handles histamine. I’ll also talk about what nutritional strategies are available along with dietary tips you can implement easily.
But first, let’s begin with the basics.
What is histamine?
 Histamine [2-(4-imidazolyl)-ethylamine] is an amine produced by various cells including mast cells, basophils, histaminergic neurons, platelets, and gastric enterochromaffin cells.
Histamine [2-(4-imidazolyl)-ethylamine] is an amine produced by various cells including mast cells, basophils, histaminergic neurons, platelets, and gastric enterochromaffin cells.
Histamine is also found in various amounts in foods containing the amino acid histidine. Fermentation, curing, and slow cooking, convert histidine to histamine thereby increasing the food’s histamine content.
Physiological functions of histamine
Let’s say you’ve been bitten by an insect. Your immune system will ‘see’ the insect’s venom and respond by triggering mast cells, a type of white blood cells which act as the guards of our innate immune system.
These mast cells will then trigger the release of histamine from storage sacs known as secretory granules.[1]
Since histamine is a signaling molecule widely distributed throughout the body, it relays information between cells in the body via four types of receptors namely H1, H2, H3, and H4 receptors. And in doing so, histamine triggers the release of other immune cells while also dilating capillaries, causing swelling.
This swelling increases the capillaries’ permeability to immune cells, enabling them to rapidly find the invader (the insect’s venom in this case) and attack it so that it doesn’t have time to cause serious adverse effects.
Histamine’s other functions in the body
Since histamine acts via four different receptors, its role goes much beyond the production of an immune response.
For instance, histamine also acts as a neurotransmitter in the brain and research suggests that it can control whole brain activity.[2] Issues with the H1 receptor could cause defective locomotor and exploratory behaviors.
Moreover, histamine is also involved in:
The body is usually well-equipped to prevent the build-up of histamine
Usually, once histamine has done its job (or after consuming a histamine-rich food), this amine will be enzymatically degraded via:[5]
- Oxidative deamination by diamine oxidase (DAO) into imidazole acetaldehyde
- Methylation by histamine N-methyltransferase (HNMT) into N4-methylhistamine
However, in some cases, the body may be unable to deal with the histamine produced or consumed.
When histamine goes haywire
 There are three main types of histamine problems:
There are three main types of histamine problems:
1. Mastocytosis
This is a rare genetic condition caused by an excess of altered mast cells. And the more mast cells a person has, the more histamine the body will produce.[6]
2. Food-induced histaminosis
More commonly referred to as histamine intolerance, food-induced histaminosis is not a true food intolerance since it stems from the body’s inability to clear out the ingested histamine.[7]
Although some foods are naturally richer in histidine/histamine, symptoms of histamine intolerance are caused by defects in the processing and elimination of histamine along with gut issues.
3. Mast Cell Activation Syndrome (MCAS)
MCAS is different from an intolerance caused by histamine consumption: it refers to an immunologic condition where the mast cells set off a hyper response to a threat.
This exaggerated reaction then leads to the release of an excess of histamine (as well as other chemical mediators like cytokines, prostaglandins, and interleukins), causing various symptoms as shown below. Put simply, MCAS is a reaction to the histamine released by the mast cells.
Common symptoms of MCAS
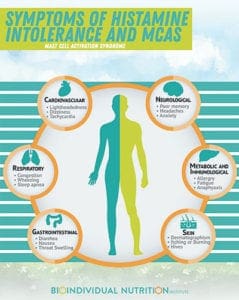 Since mast cells and their receptors are found throughout the body, MCAS can affect any organ system. For instance, MCAS can cause distress in the:
Since mast cells and their receptors are found throughout the body, MCAS can affect any organ system. For instance, MCAS can cause distress in the:
- Central and peripheral nervous systems
- Reproductive system
- Respiratory system
- Digestive system
- Immune system
As you can imagine, histamine intolerance and MCAS causes a constellation of symptoms depending on which body systems are affected.
- Headaches and migraines
- Anxiety and/ or depression
- Sleep disturbances
- “Brain fog”
- GI distress, heartburn, diarrhea
- Redness, flushing or hives
- Wheezing or shortness of breath
- Nasal congestion or drip
- Vertigo
- Arrhythmia
- Anaphylaxis
- Hypotonia and hypertension
- Circadian rhythm imbalance
- Dysmenorrhea
- Heart palpitations
- Food and chemical sensitivities
What can trigger MCAS?
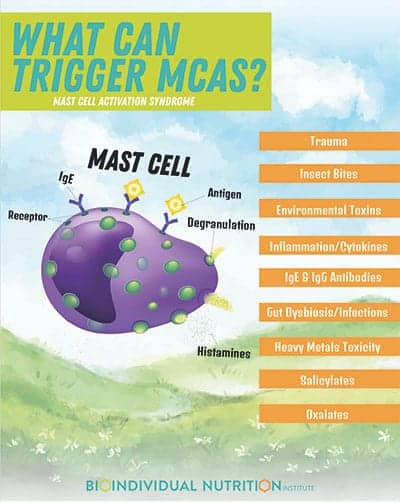 Mast cells can become overactive due to:
Mast cells can become overactive due to:
- Pollen
- Trauma
- Insect bites
- Environmental toxins
- Inflammation or cytokines
- IgE and IgG antibodies – Any type of food allergens and food sensitivities can trigger MCAS.
- Gut dysbiosis or infections caused by bacteria, viruses, fungi, Lyme, and mold.[8] The toxins released by those organisms can cause severe symptoms by (i) triggering MCAS and (ii) inducing inflammation and oxidative stress.
- Toxicity of heavy metals such as aluminum and mercury.[9]
- Salicylates (one type of phenol) – It is estimated that 0.6 to 2.5% of the population is sensitive to salicylates which can over-activate mast cells. The mast cells then release inflammatory molecules known as cysteinyl leukotrienes which then lead to various symptoms.[10]
- Oxalates – Oxalates appear to also trigger MCAS; although, this is mostly clinical evidence at this point.
Conditions associated with MCAS
In addition to the symptoms listed earlier, the following conditions are associated with MCAS, including autism and autoimmune disorders:
- Autism
- Allergies and Asthma
- Food Allergy and Intolerance
- Eosinophilic Esophagitis
- Chronic Fatigue Syndrome
- Multiple Chemical Sensitivity
- CIRS (Chronic Inflammatory Response Syndrome)
- POTS (Postural Orthostatic Tachycardia Syndrome)
- Autoimmune disorders (Hashimoto’s thyroiditis, lupus, etc.)
- Fibromyalgia
- Celiac Disease
- Irritable Bowel Syndrome
- GERD
- Interstitial Cystitis
- Migraines
- Anxiety
- Depression
- Sleeping Disturbances
Now that you know what MCAS is and how it can be triggered, let’s look at why some individuals have issues with histamine.
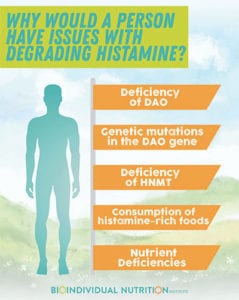
Why would a person have issues with degrading histamine?
Well, this may stem from various factors:[7]
- A deficiency of DAO secondary to a genetic issue with DAO production (more common among people of Asian origin), gluten intolerance, and inflammation. Since DAO degrades histamine, a deficiency would cause histamine to build up in the body.
Moreover, drugs like NSAIDs, antihistamines, H2-blockers, antidepressants, immune modulators, and antiarrhythmics can also adversely affect the body’s DAO levels.
- Genetic mutations in the DAO gene – These would reduce DAO’s efficiency in clearing out histamine.
- A deficiency, or reduced activity, of HNMT – This can be caused by micronutrient deficiencies (such as deficiencies of vitamins B1, B2, B12, B6, and minerals like folate, zinc, and copper). These nutritional deficiencies impact the methylation pathway via which HNMT degrades histamine.
- Consumption of histamine-rich foods or foods that naturally block DAO – This can trigger, or worsen, symptoms in individuals suffering from histamine intolerance especially if they have issues with DAO or HNMT.
- Nutrient deficiencies – Sufficient vitamin B6 and copper are required for DAO production. Nutrient deficiencies can be caused by suboptimal digestive function, higher nutrient demands (such as in cases of stress, anxiety, or poor sleep quality), and a nutrient-poor diet.
The gut’s role in MCAS
As you’re probably aware, an unhealthy gut will increase risks of MCAS. For instance, increased intestinal permeability can cause a DAO deficiency which could then lead to histamine buildup in the body.
Moreover, histamine can be produced by pathogens and beneficial bacteria. Pathogens can also produce phenols – usually, the body is able to metabolize excess phenols. However, if someone has gut issues or inadequate levels of sulfate and liver enzymes, excess phenols can trigger histamine release.
MCAS and autism – is there a link?
Definitely!
You see, the brain also has mast cells – these are close to the neurons and microglia and are mostly found in the hypothalamus which is involved in behavior and language regulation.[11]
It is well known that children with ASD are more sensitive to stress. And research by Dr. Theoharides shows that, in ASD, brain mast cells can be excessively activated by stress[12] leading to increased serum levels of neurotensin along with excess hypothalamic release of corticotropin-releasing factor (CRF).[13] (Allergens, toxins, and environmental, immune and neurohormonal triggers can also cause the brain mast cells to be overly activated in ASD.)
Now, both neurotensin and CRF stimulate mast cells to produce inflammatory and neurotoxic components that adversely affect the blood-brain barrier and cause inflammation in the brain.[11]
Neurotensin also causes the mast cells to secrete mitochondrial DNA which can act as an innate pathogen that activates immune cells, including mast cells, thus causing autoinflammation.[12] Dr. Theoharides suggests that the inflammation induced by brain mast cells could drive headaches, ‘brain fog’, and other neurological symptoms associated with ASD.[11]
What about salicylates?
Salicylate sensitivities are even more prevalent among individuals with autism and ADHD. Research suggests that individuals with autism and known food/chemical intolerances are deficient in phenol-sulfotransferase-P enzyme and/or have limited capacity to oxidize sulfur compounds.[14]
Since phenol-sulfotransferase-P enzyme metabolizes phenols, amines, and some drugs, inadequate levels of this enzyme could lead to:
- A build-up of phenols after exposure to foods and chemicals that contain phenols. This could then trigger MCAS.
- Unpleasant reactions to medications such as antibiotics or sedatives and worsening of autism symptoms in some cases.
- An accumulation of serotonin, dopamine, and serotonin. If these neurotransmitters are then further metabolized, it could result in the production of toxins which could impact sensory functions in ASD.
So, how can you identify MCAS? Well, there are various ways to test for this.
Testing for MCAS
1. Dietary Trial
A histamine trial involves the elimination of:
- Foods rich in histamine
- Foods that release histamine
- DAO enzyme inhibitors such as alcohol, tea (black, green, mate), and various energy drinks
Foods rich in histamine
- Fermented foods: sauerkraut, kombucha, fermented dairy including yogurt, kefir, sour cream, soy sauce, fish sauce
- Vinegar and Vinegar-containing foods: pickles, olives, mustard
- Cured meats: bacon, salami, hot dogs, sausage
- Aged, dried, jerky, smoked and less fresh meat and fish, as well as anchovies and mackerel
- Aged cheese
- Nuts: Peanuts, walnuts, and cashews
- Vegetables: avocados, mushrooms, eggplant, spinach, and dried tomatoes and tomato sauce
- Dried fruit and citrus fruits
- Long/slow simmered and roasted foods: such as bone broths and pot roast
- Fermented alcohol: wine, beer, brandy, port, sherry, rum, champagne
- Probiotic supplements
Foods that release histamine
- Bananas
- Chocolate
- Alcohol
- Milk
- Nuts and peanuts
- Fruit: Papaya, Pineapple, Strawberries
- Tomatoes
- Shellfish
- Artificial preservatives and dyes
Note: Any diet can be high in histamine depending on which foods are included. So just because a diet is a therapeutic one, it does not mean that it is suitable for everyone.
For instance, the GAPS diet, especially the beginning phases, can be particularly high in histamine since these phases include lots of bone broth, fermented foods, and slow simmered meats. This is not limited to a GAPS diet. And any individual diet that includes large amounts of these foods would be a high histamine diet. This being said, with some awareness and attention, most diets can be adapted to be low in histamine.
2. Lab tests[12]
- Serum tryptase – This is usually the test that some functional medicine doctors used to diagnose MCAS
- Plasma heparin
- Plasma histamine
- N-methylhistamine
- Plasma prostaglandin D2 (plasma PGD2) – NSAIDs are to be avoided for at least 5 days before testing since they can reduce plasma PGD2 levels
- Urine prostaglandine D2 (urine PGD2) –
- PGF2a
- Serum chromogranin A – Proton pump inhibitors must be avoided at least 5 days before testing since they will interfere with test results.
You could also look at genetic SNPs for DAO and HNMT – mutations in HNMT have been shown to result in high levels of histamine in the brain.[15] This could lead to intellectual disability.
A high histamine to DAO ratio could mean that:
- Dietary histamine intake is excessive (if currently on a regular diet)
- Gut dysbiosis is causing over-production of histamine (if currently on a low histamine diet)
- The body is unable to maintain optimal DAO levels
If histamine levels are normal but DAO levels are inadequate, this could indicate a genetic DAO deficiency.
3. Supplement challenge
If you are unable to test your histamine and DAO levels, you could try a supplement challenge. This involves consuming a low histamine diet while taking a DAO supplement at each meal. If your symptoms improve, this could indicate that your DAO levels are low.
What can you do about MCAS?
1. Try a low histamine diet
The following foods are low in histamine.
- Fresh meats
- Fresh fish
- Vegetables (except spinach, pickles, olives, eggplant, mushrooms)
- Fruits (except bananas, papaya, pineapple, strawberries, citrus, dried fruit, tomato sauce)
- Beans
- Gluten-free grains
- Butter and ghee
2. Look into supplementation support with your practitioner
Some supplements that can help:
- DAO enzymes
- Mast cell stabilizers and anti-histamines
- Quercetin
- Luteolin (product:Neuroprotek)
- Prickly pear
- Vitamin C
- B6
- Omega-3 fatty acids (prostaglandins)
- Alpha Lipoic Acid
- Methylating Nutrients
- Methyl B12, Methyl Folate, zinc, magnesium, riboflavin, B6/P5P, choline, SAM
- And foods rich in them
- Probiotics that can decrease histamine
- bifidobacter species
Remember Dr. Theoharides’ research? Well, he created Neuroprotek, a nutritional supplement that contains natural flavonoids, like luteolin and quercetin. These antioxidants can reduce inflammation by inhibiting the release of inflammatory mediators from mast cells. The supplement also contains rutin and quercetin – these act “as ‘decoys’ to keep the intestinal and liver enzymes occupied to allow luteolin to escape metabolism and reach the brain”.[17]
3. Avoid high histamine supplements
These include:
- Probiotics like Lactobacillus Casei and Lactobacillus Bulgaricus since these increase histamine levels.
- Fish oil supplements are a bit tricky in that they can help reduce salicylate intolerance and prostaglandins (which cause inflammation) but they are high in amines. So, you may want to start with diet first and then add in the low-histamine supplements mentioned earlier. Then, with the guidance of your healthcare professional, you could include fish oil. If symptoms improve, then you could keep the fish oil supplements. However, you may need to remove these supplements if you notice that symptoms worsen.
- NAC since it can block intestinal DAO although it does have some benefits. Again, you may want to assess tolerance.
Troubleshooting
You’ve tried avoiding foods rich in histamine and those that release histamine, but symptoms persist?
Then, you might want to look into:
- Cooking methods – To reduce histamine content of broths, you’ll want to select bones with the meat and simmer the broth for a short period. You may also want to avoid slow cooked foods as well as those that are marinated, fermented, or cured. Also, if possible, consume fresh meat instead of frozen ones and avoid leftovers.
- The Failsafe Diet – this trial diet, which I’ve previously discussed here, eliminates amines, phenols, and glutamate.
- The low-oxalate diet – You can find out more about this diet in my video or article. Check out these recipes for easy ideas.
Now I’d like to hear from you: have you dealt with MCAS? What helped you?


